How to Open a Group Home in Georgia
Coronavirus: Why some racial groups are more vulnerable
(Image credit:
Getty Images
)

From discrimination to language, a variety of factors are affecting different groups' vulnerability to coronavirus — with sometimes devastating results.
E
Even with a virus that doesn't respect borders, vulnerability is spread unevenly. And some of the largest disparities seen so far have involved race and ethnicity.
Early data of the Covid-19 crisis, broken down by race, is alarming. In the US, in Chicago, as of early April 2020, 72% of people who died of coronavirus were black, although only one-third of the city's population is. In Georgia, as of 17 April, white people accounted for 40% of Covid-19 cases where race was reported, although they represent 58% of the state. In the UK, of the first 2,249 patients with confirmed Covid-19, 35% were non-white. This is much higher than the proportion of non-white people in England and Wales – 14%, according to the most recent census.
You might also like:
- Why Covid-19 is different for men and women
- What is Covid-19's real death rate?
- How the new coronavirus might change the world
Given the long history of unequal health outcomes, these patterns shouldn't be surprising. The pandemic is the latest example of how racial dynamics play out in complex – and still not entirely understood – ways.
Income inequality
In many majority-white countries like the US (as well as some minority-white countries like South Africa), people from other ethnic and racial groups have less access to economic resources – whether that means high-earning jobs or a full pantry. That economic vulnerability often translates to poorer health outcomes.

People wait in line at a food bank in Van Nuys, California, where organisers said they had distributed food for 1,500 families amid the spread of Covid-19 (Credit: Getty Images)
There are a number of consequences of lacking access to consistent nutrition, including higher risk of underlying health conditions. In the US, for example, African Americans are more likely than white residents to have diabetes, heart disease and hypertension – which weaken lungs and immune systems. And people with pre-existing health conditions are more likely to develop severe Covid-19 symptoms.
Of course, this doesn't just mean certain groups are more vulnerable to Covid-19. It also means they're more vulnerable to its economic consequences. In South Africa, for example, development economist at the University of Witwatersrand Imraan Valodia has forecast that the lockdown will lead to a 45% loss of income for the poorest 10% of households, with especially harmful effects on informal workers without a safety net. As a result, he is calling for an end to the lockdown (one alternative could be a curfew).
"For the upper classes who can continue to earn an income and who have wealth to fall back on, the lockdown is easy to manage. For the lower classes, this is not the case," Valodia says.
Other racial disparities
But economic inequality isn't the only challenge disproportionately faced by BAME (Black, Asian and Minority Ethnic) groups.
Persistent environmental injustice, for example, means that disproportionately high numbers of ethnic-minority households in North America and Europe live near incinerators and landfills, and schools with high proportions of minority students are located near highways and industrial sites – for both economic and non-economic reasons. This too affects vulnerability to lung-inflaming conditions like asthma and Covid-19. "Air quality, which early data is highlighting to be a potential risk factor for Covid-19, is also a risk factor for respiratory health," says Grania Brigden, who leads the tuberculosis department at the lung health organisation The Union.

An army sergeant speaks to a patient at the Javits New York Medical Station, which supports local hospitals in New York City (Credit: Getty Images)
Then there is racism itself. Allostatic load (or "weathering") refers to the accumulated physiological burden from the stresses caused by racism and race-related disadvantage, such as the frequent secretion of stress hormones.
While weathering is more severe for people with low socioeconomic status, studies suggest that it affects the health deterioration and mortality of higher-income African Americans (especially women) as well, including their newborns.
Even medical staff themselves may not be shielded from these effects: investigation is ongoing into why the first 10 doctors in the UK reported to have died from Covid-19 were all BAME.
Occupational factors
Meanwhile, around the world, certain racial and ethnic groups are disproportionately represented in at-risk professions. For instance, 26.4% of Transport for London staff are from BAME groups (vs. the 14% for all of England and Wales). People of colour are also substantially more likely to be unemployed, underemployed or precariously employed, which makes them especially likely to undertake hazardous temporary or gig economy work like delivering food.

A police official warns labourers to wear face masks at the grain market in Chandigarh, India (Credit: Getty Images)
In the US, farmworkers are often undocumented migrants from Latin America with little control over safe working conditions. It can be difficult to ensure physical distancing in the fields, isolation in the farmworker camps, or proximity to medical facilities. Farmworkers in the US have high rates of diabetes and pesticide exposure, stressing their immune systems and thus making them more vulnerable to infectious diseases. Wael Elamin, a medical microbiologist at King's College Hospital in Dubai, points out that migrant workers also face overcrowded living conditions in a number of Middle Eastern countries that depend on their labour.
In general, undocumented people are especially unlikely to seek formal medical care out of fear of being reported to law enforcement. This influenced Portugal's decision to grant temporary residency rights to asylum seekers and other migrants whose residency applications were pending: minimising that fear would help public health. It's still too early to know whether this decision has paid off, but public health agencies have praised the move.
Housing differences
Overcrowding also is likelier to affect lower-income groups across the globe, from Native American families to displaced Rohingyas. With a disease as infectious as Covid-19, it's easy to see how that could translate to poorer outcomes.
In a Population Council phone survey of five informal settlements in Nairobi, for example, 85% of respondents reported that they had no place in their home to isolate an ill person, 82% would be unable to stay at home for 14 days (mainly due to the loss of income), and 37% would have difficulty washing their hands frequently due to a lack of water.
In the UK, meanwhile, one survey found that 26% of Bangladeshi British households, and 21% of black African ones, have more people than bedrooms. The same is true of just 2% of white British households. Bangladeshi, Indian and Chinese households in the UK also have higher rates of elderly people living with children – a clear vector for passing on Covid-19 to the most vulnerable age group.
Precarious housing is another challenge, as people who are homeless or vulnerably housed are less able to observe social distancing and self-isolation. In the UK, at least 31% of homeless households prioritised for assistance are non-white (although, as we've seen, non-whites make up just 14% of the overall population of England and Wales). Demolitions of shack settlements have continued in Durban, South Africa despite the public health crisis. Nigerians are being targeted for eviction in Guangzhou, China. And black women in Milwaukee and other US cities are much more likely than white residents to rent their homes (and to be evicted from them, although evictions have been suspended in Milwaukee County in response to the crisis).

In Rio de Janeiro, a person who is homeless eats food provided by residents of the Chapeu Mangueira slum during the Covid-19 outbreak (Credit: Getty Images)
It's important to remember that residential segregation isn't simply a by-product of income inequality. It's also a result of systematic and widespread housing discrimination on the basis of race, caste and other identity-linked factors.
Cultural factors
At the same time, the crisis is amplifying misinformation and biases against specific groups.
It has boosted Islamophobia in India, thanks in part to "corona jihad" rumours on social media about Muslims deliberately coughing and sneezing on others. The US has also seen rumours, especially during the early part of the epidemic, about black people being somehow immune to the virus – a myth that persists across Africa as well.
Biases also mean some are less likely to take preventative behaviour like wearing masks. Black men in the US have reported being uncomfortable wearing masks in public: racial bias and profiling means they're more likely to be seen as a criminal or dangerous, rather than as simply protecting their own health.
Then there is the impact on Asians and Asian Americans.

Members of the Asian American Commission hold a press conference condemning racism towards the Asian American community during the Covid-19 crisis (Credit: Getty Images)
Cynthia Choi is one of the executive directors of Chinese for Affirmative Action. This organisation, along with the Asian Pacific Policy and Planning Council, launched the Stop AAPI Hate website on 19 March 2020. The site collects reports of harassment and assault of Asians and Pacific Islanders in the US, including incidents of Asian Americans being physically assaulted and coughed and spat on. Most of the people targeted in these incidents have been women.
"AAPIs are becoming increasingly fearful of being harassed or attacked going to work, walking in their neighbourhoods and going to public places," Choi says, based on the incident descriptions received by Stop AAPI Hate.
Language barriers
Even language has had a marginalising effect on some groups around the world.
Much of the initial public health guidance around Covid-19 has been in dominant languages, points out Salman Waqar, an academic GP registrar at the University of Oxford and the general secretary of the British Islamic Medical Association. "There needed to be a better understanding at the beginning of this pandemic that these messages may not necessarily get through to the grassroots," he says.
Indeed, terms like "social distancing" and messages about safety measures have been difficult to translate into a number of languages.
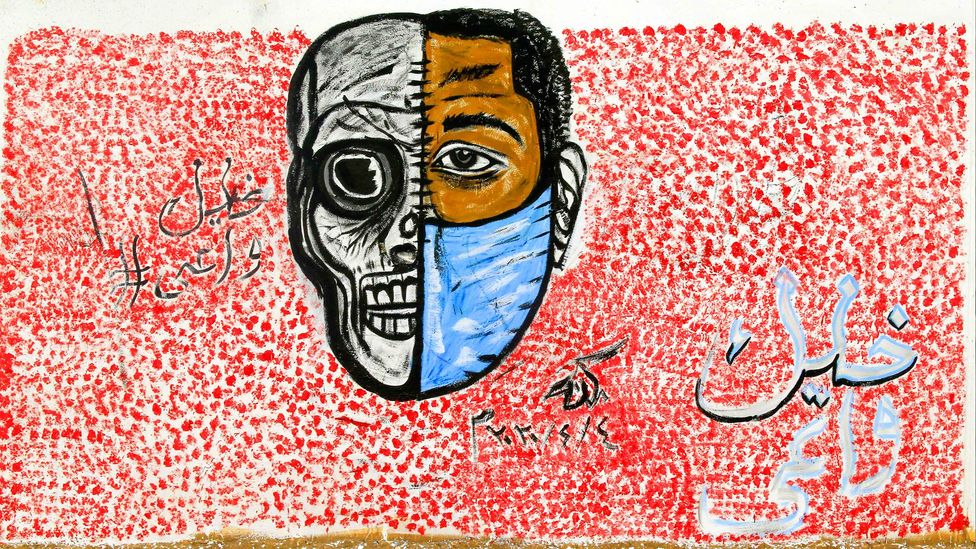
Urban art depicting the importance of face masks, part of a Covid-19 campaign, is pictured with the Arabic hashtag 'Stay aware' in Khartoum (Credit: Getty Images)
You only need to look at the Ebola outbreak that started in the Democratic Republic of Congo in 2018 to see what effect this can have, notes Ellie Kemp, head of crisis response for Translators without Borders. For instance, official communications from the Ministry of Health and the World Health Organization likely started out in either English or French, then were translated into a non-local version of Swahili, with key terms like "swab" remaining in French.
"One of the net results of the confusion that caused was that people didn't really trust the information," Kemp says. Women and less educated people, especially, "didn't understand the language used by the doctors and the medical staff. And so they didn't feel they were able to make themselves understood." Many chose not to seek medical care, or were misdiagnosed.
"There's this terrible coincidence between people who are likely to have less health literacy to start with, and people who are less likely to speak an international language," Kemp says.
She remembers widespread puzzlement about the term "contact tracing". People didn't know what a "contact" meant – was it someone in your phone book? Sexual contact?
The phrase was ultimately translated into a Swahili version of "monitoring people who've been close to a sick person" – a term that was easier to understand.
Narrowing the gaps
Experts say that addressing these disparities in the short term will require steps that will help everyone, but especially people of colour: getting protective equipment to all essential workers, including janitors and sanitation workers; increasing access to medical care, whether in private or public facilities; providing secure housing for people who fall ill; increasing financial support to both individuals and nonprofit organisations; and ensuring the basics, like handwashing stands and soap, in the areas with the fewest resources, including informal settlements and refugee camps.

A boy washes at the Dibege Refugee Camp in Iraq; ensuring that there are handwashing stands and soap is key to fighting Covid-19's spread in refugee camps (Credit: Getty Images)
Getting vitamin D supplements to vulnerable groups, including darker-skinned people, could help with immune response in general (although there isn't a consensus about how widespread vitamin D supplementation should be, and in which amounts).
There's also an urgent need for more data, broken down by demographic groups, to know how to best serve different communities. But this has been stymied by political obstacles in some countries, and insufficient resources in others. As of 14 April 2020, only 22% of Covid-19 cases reported in the US specified the race of the patient. And microbiologist Elamin points out that in Sudan, it's challenging to collect medical data on whether, for instance, respiratory illnesses recorded in December 2019 and January 2020 could have been cases of Covid-19. Gathering more specific demographic information on population groups most affected would be even tougher and more sensitive.
Attention to the medium and longer term will also be needed. The pandemic highlights and exacerbates health inequities, but it doesn't create them. Nor will the disparities end with the emergency.
As a result, say experts, policy discussions around social protection and universal healthcare are more important now than ever. According to lung health expert Brigden, the pandemic "has highlighted, even in higher-income countries, the importance of a strong and well-funded health system that is available to all".
The world also needs an acceleration of environmental regulations that reduce air pollution (which particularly weakens respiratory health among marginalised communities); the US is currently seeing a rollback, instead.

A roadside tailor stitches cloths in heavy smog in New Delhi, India; air pollution is linked to weakened respiratory health (Credit: Getty Images)
And there needs to be a careful look at how economic fallout will disproportionately impact BAME communities. For example, after the 2007-08 financial crisis, ethnic minorities in the UK faced higher unemployment, lower earnings and higher housing costs.
"What's going to kill us more: the bug, or the poverty that's associated with the bug?" asks microbiologist Elamin.
For now, it's impossible to answer. But what is clear regarding coronavirus is that, as he says, "the way it spreads is not equal".
But there is a best-case scenario. And that is that the current pandemic will galvanise more, and longer-lasting, attention to the social, political and economic structures that shape how different people experience the pandemic – and spur action so that, in the future, a factor like an individual's race or ethnicity will have less impact on the risk to their lives.
As an award-winning science site, BBC Future is committed to bringing you evidence-based analysis and myth-busting stories around the new coronavirus. You can read more of our Covid-19 coverage here .
--
Join one million Future fans by liking us on Facebook , or follow us on Twitter or Instagram .
If you liked this story, sign up for the weekly bbc.com features newsletter , called "The Essential List". A handpicked selection of stories from BBC Future, Culture, Worklife, and Travel, delivered to your inbox every Friday.
How to Open a Group Home in Georgia
Source: https://www.bbc.com/future/article/20200420-coronavirus-why-some-racial-groups-are-more-vulnerable
0 Response to "How to Open a Group Home in Georgia"
Post a Comment